Transpalpebral tonometer for intraocular pressure measuring
Eye diseases department of the Russian State Medical University medical faculty, Moscow
Eye tonometry is one of the leading methods used in the patient with ophthalmopathology checkup. The first tonometer acceptable for clinical practice was designed and described in 1884 by A.N.Maklakov [2]. The tonometers introduced earlier had serious drawbacks and were not used in clinical practice. Before this the intraocular pressure (IOP) was evaluated only approximately with the help of eye palpation through the upper eyelid. At present palpation method is still widely used in clinical practice. Using it a skilled ophthalmologist can evaluate approximately whether ophthalmotone is normal (Tn), increased (T+1, T+2) or decreased (T-1, T-2), distinguish normotension from hyper- or hypotension. The palpation method suffers from subjectivism, uncertainty of results at ophthalmotone moderate change but at the same time it shows the principle possibility of transpalpebral tonometry.
Intraocular pressure
The eyeball is a reservoir of the spherical form, filled with fluid, incompressible contents. IOP is caused by the influence of the elastic forces, arising in eye coverings while they are being stretching.
IOP level is determined by watery moisture (WM) circulation in an eye and by pressure in episclera veins [3]:
PO=F/C+Pv,
where PO - IOP; F - WM minute volume; C - coefficient of easiness of WM flow-out from an eye, Pv - pressure in episclera veins.
IOP increases while moving from vertical to horizontal position and especially in Trendelenburg position and while squeezing the neck's veins because of the pressure increasing in episclera veins (Pv) [4].
IOP is a dynamic, continuously changing value. They distinguish its system, rhythmic fluctuations around relatively constant level and momentary changes of casual character. IOP fluctuations around the level depend on changes in bloodfilling of intraocular vessels and on outer pressure on the eyeball.
There are 3 types of rhythmic IOP fluctuations around the level [3]:
- eye pulse (from 0,5 to 2,5 mm Hg),
- respiratory waves ( from 0 to 1 mm Hg),
- Hering-Traube waves (from 0 to 2,5 mm Hg).
The successive measurings of IOP in the same eye with a tonometer vary from each other mainly due to the ophthalmotone rhythmic fluctuations. Winking, pressing of the eye with orbicular muscle or external muscles of the eyeball momentary increase IOP, provide eye massage and decrease venous congestion. At the same time changes of orbicular and transpalpebral muscles tone during tonometry are often the cause of error while measuring IOP level.
Statistically normal IOP varies from 9 to 21 mm Hg (on average 15-16 mm Hg). It has daily and seasonal fluctuations. The IOP distribution in the normal population is asymmetrical (splayed to the right). In middle age the distribution asymmetry increased. More than 3% of healthy persons have IOP above 21 mm Hg [4]. The ophthalmotone measuring accuracy in the area of the normal and reasonably increased (up to 30 mm Hg) IOP is especially important for a practical doctor.
Intraocular pressure regulation
Each eye is adjusted to a certain IOP level (balance pressure) which is supported by passive and active mechanisms. IOP being increased pressure of moisture flow-out and filtration from an eye increased, WM production being decreased its flow-out decreased and the balance pressure restores.
Active mechanisms of IOP regulation have been not enough studied. Collaboration of hypothalamus, adrenal glands, vegetative nervous system and local autoregulatory mechanisms is possible.
Opthalmotonometry
The IOP measuring is based on the eyeball deformation under the influence of an outer effect. At that the values of deformation (S), the force (W) influencing the eye and IOP (Pt) as a first approximation are connected with each other with the following dependence [5]: Pt = f(W/ S). All tonometers fall into devices: 1) with constant and variable pressure force on the eye, 2) with constant and variable value of eye deformation, 3) corneal, scleral and transpalpebral, (4) applanation, impression and ballistic.
Ophthalmotonometers used in the Russian Federation
- Maklakov tonometer and Filatov-Kalve elastotonometer.
- Goldmann applanation tonometer (reference)
- Perkins and Dregger applanation tonometers
- Grolman non-contact applanation tonometer, 1972
- Schiotz impression tonometer
- diaton transpalpebral tonometer
All the tonometers mentioned above (besides diaton) measure IOP through cornea.
Advantages and disadvantages of corneal tonometry
It is possible to note the following advantages of corneal tonometry: 1) it is more accessible for tonometry on an open eye then sclera; 2) between tonometer and eye cavity there's no other structures interposition (conjunctiva, eyelid, ciliar body), but cornea; 3) cornea's individual size, thickness and crookedness are less different in comparison to other parts of eye fibrous membrane.
At the same time corneal tonometry has serious drawbacks:
- Cornea has high pain sensitivity and the tonometry is impossible without prior anesthesia, which in some patients causes conjunctiva irritation, hypostasis of cornea epithelium, short-term IOP increasing, and allergic conjunctivitis.
- Cornea has regular spherical shape only in the central zone and flattens towards periphery; its thickness increases from 0,5-0,6 mm in the center to 0,8 in the periphery. Besides, the existent individual peculiarities both in cornea's crookedness and thickness influence significantly on the tonometry results [6, 12].
- During the corneal tonometry it is very difficult to prevent the increasing of orbicular and palpebral muscles tone, that leads to IOP increasing. The ophthalmotone increasing may be also connected with the blood pressure increasing during the tonometer's bringing near the open eye [3].
- It is known that a tear may contain bacteria and dangerous viruses (hepatitis B virus, herpes, adenoviruses, AIDS). But the problem of tonometers sterilization is far from perfection [11].
- The corneal tonometry is contraindicative in eyelids and cornea edema, nystagmus, conjunctivitis, corneal erosions, keratitis, hypostasis and sores.
Diaton tonometer - basic principles
Transpalpebral ophthalmic tonometer (diaton) was designed by a group of ophthalmologists and engineers. There was the task to design portable and simple in use device, which could provide IOP measuring through the eyelid not only in ophthalmology studies but at home as well. It should possess enough accuracy, quick operation and provide the possibility to carry out ophthalmotone monitoring that is very important both for glaucoma diagnostics and for controlling the effectiveness of treatment. "Digital Portable Tonometer of Ocular Pressure" (diaton) designed by us fulfills all these tasks (fig.1).
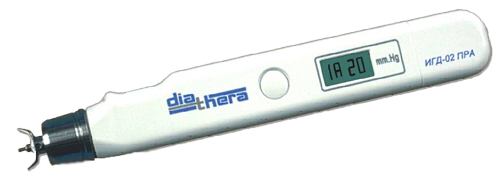
Fig.1
The peculiarities of the new tonometer are that IOP measuring is realized through the eyelid that excludes contact with conjunctiva and cornea and does not require anesthetics application.
At that the mechanical influence on the eye is realized through the eyelid on sclera. The tonometer's position while measuring IOP is shown on fig.2.

Fig.2
The measuring principal of the new tonometer is based on processing the rod movement resulting from its free fall and interaction with the elastic surface of the eye to be measured. The main problem was how to exclude the influence of an eyelid individual peculiarities on the tonometry results. This was solved by pressing the eyelid on the area with the diameter of 1,5 mm to such extent that the pressed area of the lead acts like a rigid transfer link while the rod interacts with the eye at the same time excluding the painful sensation. This method of compensating the eyelid influence led to the choose of dynamic (ballistic) way of dosated mechanical influence on the eye for evaluating its elastic peculiarities.
To determine the position in the process of its free fall from the constant height and the interaction with eye through the eyelid the device has position sensor. Value of the points of the rod movement function in time is remembered by the built-in processor. In diagram form the function of the rod movement in time is shown in fig.3.
Fig.3 Function of the rod movement in time:
H - change in the rod position during the free fall, t - time after the fall starting, B - minimum point of the rod movement function.
For point B the following equation is true: P=F/S, where P - IOP, F - eye elasticity force, influencing the rod, S - the area of eye and rod interaction (area of its square). According to Newton's second law: F=m*a, where m - the rod's weight, a - the rod's acceleration while interacting with the eye elastic surface. Then P=m*a/S. The rod's weight and the interacting area - S are constants So to evaluate P it is enough to measure the rod movement acceleration (a) in point B.
Errors of IOP measuring
In clinical practice it is customary to evaluate errors of IOP measuring with the new tonometers in comparison with the results received in the same eyes with Goldman tonometer (Reference tonometer) and taking into consideration scatter of data received during repeated measurings with the same tonometer [8].
Numerous studies carried out in hundreds of patients during several years show high reliability of IOP measurings with diaton tonometer. Scatter of results received using the new tonometer and Goldman tonometer had no systematic character and did not exceed 4 mm Hg. In repeated IOP measurings in healthy eyes the displays fluctuations were in the range 2-4 mm Hg [1]. According to the literature data the scatter of results while carrying out the repeated measurings using Goldman tonometer is 2-3 mm Hg in healthy eyes [10]. While checking various samples of Goldman tonometers produced in lots it is found the systematic difference of the displays of 2-3 mm Hg depending on the variant of each device's double prism and spring calibration. Eye refraction, astigmatism, cornea's crookedness and thickness, width of the moisture ring around the flattening area, hyper- or hypofluorescence of the ring [6, 7, 9]. As it was mentioned above, the error of IOP level measuring depends on the character and value of ophthalmotone rhythmic and casual fluctuations as well as on the tonometrist's skill.
The experience of operating diaton and Goldman tonometers shows that their displays have good correlation.
Diaton tonometer has accuracy enough for clinical purposes, requires no anesthetics and sterilization. Besides, they are safe (can not damage the cornea), comfortable for the patients and easy in use. They can be used not only in ophthalmology studies but at home as well.
LITERATURE
- Илларионова А.Р., Пилецкий Н.Г.//Клин.офтальмол.-2001-№2.-С.55-56
- Маклаков А.Н.//Мед.обозр.-1884.-Т.22-С.1092-1095
- Нестеров А.П., Бунин А.Я., Кацельсон Л.А. Внутриглазное давление: физиология и паталогия.-М.,1974
- Нестеров А.П. Глаукома.-М.,1995
- Goldmann H., Schmidt T.//Opthalmologica.-1957-Bd 136.-S.221-231.
- Mark H.H.//Am.J.Ophthalmol.-1973.-Vol.76-P.223-227
- .//Ibid.-1960.-Vol.49.-P.1149
- Moses R.A., Liu C.H.// Ibid.-1968.-Vol.66.-P.89-94
- Motolko M.A.//Can/J/Ophthalmol.-1982.-Vol.17.-P.93-97.
- Phelps C.D.,Phelps G.K.//Graefes.Arch.Clin.Exp.Ophthalmol.-1976.-Vol.198.-P.39-44
- Schottenstein M.H.//The Glaucomes/Eds R.Ritch et al.-St.Louis, 1996.-Vol.1.-P.407-428.
- Whitacre M.M., Stein R.A., Hassanein K.//Am.J.Ophthalmol.-1993.-Vol.115.-P.592-597